Telemedicine has quietly but permanently changed the doctor–patient relationship. What once relied on physical presence, touch, and shared space is now often built through screens, microphones, and digital platforms. As telemedicine becomes a core part of modern healthcare, doctors and patients alike are adjusting to a new form of connection—one that is faster, more accessible, but sometimes emotionally distant.
For doctors working in telehealth and virtual care, the question is no longer whether telemedicine will stay, but how telemedicine is reshaping trust, communication, and the very identity of the doctor–patient relationship.
What Telemedicine Really Changed in Healthcare
Telemedicine did more than move consultations online. It fundamentally altered how doctors and patients interact.
The traditional doctor–patient relationship was built around:
-
Physical examination
-
Face-to-face reassurance
-
Shared silence and presence
Telemedicine replaces these with:
-
Digital communication
-
History-focused decision-making
-
Technology-mediated trust
This shift has profound implications for patient satisfaction, diagnostic confidence, and professional fulfillment.
How Telemedicine Improves the Doctor–Patient Relationship
Despite common fears, telemedicine can strengthen the doctor–patient relationship when used appropriately.
Telemedicine Improves Access and Continuity of Care
Telemedicine removes geographic and logistical barriers. Patients who once delayed care now attend follow-ups more consistently. For chronic disease management, telemedicine often improves continuity and adherence, strengthening long-term trust.
Telemedicine Encourages More Open Communication
Many patients feel more relaxed during virtual doctor visits. In their own environment, patients often speak more honestly about symptoms, mental health, and lifestyle factors—key elements of effective telehealth communication.
Where Telemedicine Strains the Doctor–Patient Relationship
While telemedicine offers convenience, it also introduces real challenges.
Telemedicine Limits Physical Examination
The inability to perform hands-on examination is one of the biggest telemedicine challenges. Patients may question diagnostic accuracy, and doctors must manage increased uncertainty, relying heavily on history and clinical judgment.
Telemedicine Can Feel Transactional
Back-to-back virtual consultations can unintentionally turn care into a checklist. When telemedicine is rushed, patients may feel unheard, and doctors may feel disconnected from their professional purpose.
Telemedicine and Trust: Can Trust Be Built Without Touch?
Trust is the foundation of the doctor–patient relationship, and telemedicine forces us to redefine how trust is built.
In telemedicine, trust depends on:
-
Clear explanations
-
Active listening
-
Transparency about limitations
Patients are less concerned about physical presence than they are about feeling understood. When doctors communicate clearly and safety-net effectively, telemedicine trust can be just as strong as in-person care.
How Telemedicine Is Changing the Doctor’s Role
Telemedicine doesn’t just change patient experience—it reshapes the doctor’s role.
Telemedicine Shifts Doctors From Examiners to Interpreters
Without physical exams, doctors practicing telemedicine become expert interpreters of symptoms, risk, and probability. Clinical reasoning takes center stage.
Telemedicine Increases Cognitive and Emotional Load
Telemedicine requires sustained attention, verbal empathy, and constant decision-making under uncertainty. This contributes to telemedicine-related burnout when systems prioritize volume over quality.
When Telemedicine Works Best for the Doctor–Patient Relationship
Telemedicine is not one-size-fits-all.
Telemedicine works best for:
-
Chronic disease follow-ups
-
Mental health consultations
-
Results discussion
-
Preventive care and lifestyle counseling
Telemedicine works poorly for:
-
Acute abdominal pain
-
Neurological deficits
-
First-time complex presentations
Teaching patients when telemedicine is appropriate protects both safety and trust.
Practical Ways Doctors Can Strengthen the Doctor–Patient Relationship in Telemedicine
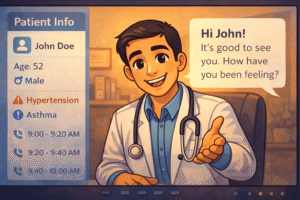
Human First, Telemedicine Second
Begin every telemedicine consultation by acknowledging the patient as a person, not a task. Small pauses, eye contact with the camera, and clear introductions matter.
Over-Communicate During Telemedicine Visits
In telemedicine, reassurance must be verbalized. Explain clinical reasoning clearly and provide explicit safety-netting to reduce patient anxiety.
Set Clear Telemedicine Expectations
Honesty builds trust. Explaining what telemedicine can and cannot do prevents dissatisfaction and reinforces professional integrity.
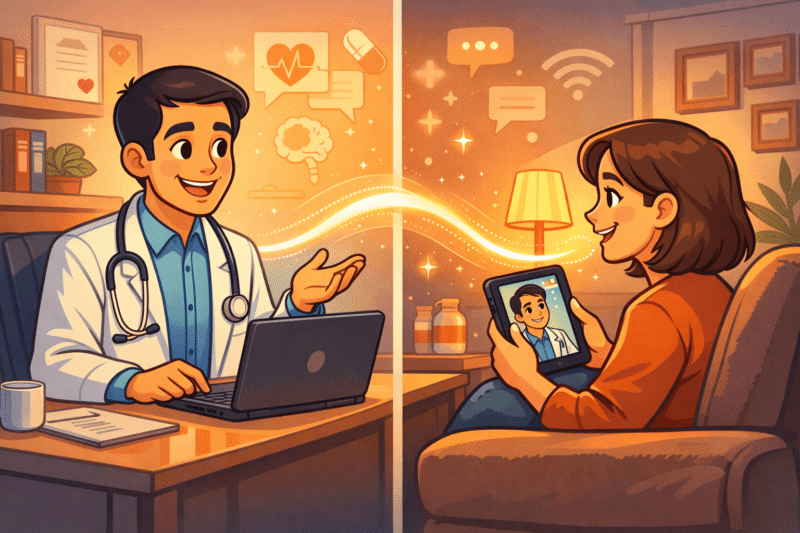
The Future of Telemedicine and the Doctor–Patient Relationship
Telemedicine is not replacing traditional care—it is creating hybrid healthcare models. According to the World Health Organization, telemedicine improves healthcare access when integrated responsibly into existing systems.
Research published in The New England Journal of Medicine highlights that patient satisfaction in telemedicine depends more on communication quality than technology itself.
The CDC also emphasizes that telehealth is most effective when combined with clear clinical guidelines and patient education.
What Telemedicine Can Never Replace
Telemedicine cannot replace:
-
Physical examination
-
Human intuition
-
Shared presence in moments of fear or grief
Technology can enhance care, but the essence of medicine remains human.
Telemedicine Does Not End the Doctor–Patient Relationship—It Redefines It
Telemedicine is changing the doctor–patient relationship, but it does not have to weaken it. When used thoughtfully, telemedicine can improve access, continuity, and trust. The responsibility lies not with the technology, but with how doctors choose to practice medicine within it.
The future of telemedicine is not about screens—it is about preserving humanity in digital care.



1 comment
Thanks for sharing Sir