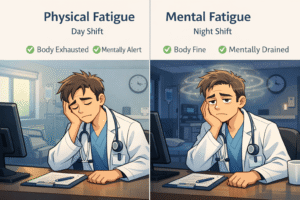
Night shifts are one of the most misunderstood stressors in medicine. Many doctors expect night shifts to be physically exhausting—long hours, fewer staff, constant interruptions. But what surprises most doctors is this: after night shifts, the body may feel fine, yet the mind feels completely depleted.
This disconnect is not a personal weakness. It is physiology. Night shifts primarily damage mental stamina, not physical endurance, and confusing the two leads doctors to recover the wrong way.
Understanding the difference between mental fatigue vs physical fatigue is critical if you want to survive night shifts without sliding into burnout.
Mental Fatigue vs Physical Fatigue: A Clear Definition for Doctors
What Is Physical Fatigue?
Physical fatigue is what most doctors expect after a demanding shift:
-
Muscle heaviness
-
Bodily exhaustion
-
Physical soreness
-
A clear sense of “I need rest”
Physical fatigue is usually proportional to workload and improves with sleep, nutrition, and time off. After day shifts or physically demanding on-call duties, recovery is predictable.
What Is Mental Fatigue?
Mental fatigue is different—and far more dangerous during night shifts.
It presents as:
-
Slowed clinical reasoning
-
Poor concentration
-
Emotional blunting or irritability
-
Decision fatigue
-
A sense that “my brain just isn’t working”
Mental fatigue affects executive function, judgment, and emotional regulation. Crucially, mental fatigue does not reliably resolve with sleep alone, especially after night shifts.
Why Night Shifts Cause More Mental Fatigue Than Physical Fatigue
Night shifts are not just late working hours. They force the brain to function at a time it is biologically programmed to rest.
Night Shifts and Circadian Rhythm Disruption
The human circadian rhythm regulates alertness, cognition, hormone release, and sleep architecture. Night shifts suppress melatonin, elevate cortisol at the wrong time, and fragment restorative sleep.
The brain remains awake, but it is operating in a biologically hostile environment.
The National Institute of General Medical Sciences explains how circadian misalignment impairs cognitive performance and decision-making.
Decision Density During Night Shifts
Night shifts often involve:
-
Fewer senior staff
-
Higher autonomy
-
Constant low-grade decision-making
-
Reduced safety buffers
Even when physical workload is low, the cognitive load remains high. This leads to decision fatigue—one of the fastest ways to drain mental energy.
Why Mental Recovery Is Poor After Night Shifts
Sleep after night shifts is usually:
-
Shorter
-
Lighter
-
Fragmented
-
Lower in REM and deep sleep
The Sleep Foundation outlines how daytime sleep fails to provide adequate cognitive recovery.
This is why doctors can sleep 7–9 hours after night shifts and still feel mentally exhausted.
Signs of Mental Fatigue After Night Shifts Doctors Often Miss
Many doctors mislabel mental fatigue as “stress” or “burnout” too early. Common signs include:
-
Slower documentation and chart review
-
Increased irritability with patients or colleagues
-
Difficulty focusing during handover
-
Overthinking simple clinical decisions
-
Emotional detachment or apathy
If you feel mentally exhausted but not physically tired, night shifts are the likely cause.
Why Sleep Alone Does Not Fix Night Shift Fatigue
Sleep Quantity vs Sleep Timing After Night Shifts
Doctors often respond to night shifts by chasing more sleep. The problem is not sleep duration—it is sleep timing.
Daytime sleep conflicts with circadian biology. Even long sleep cannot fully restore mental clarity when the brain is sleeping at the wrong time.
Mental Fatigue Accumulates Across Night Shifts
Unlike physical fatigue, mental fatigue accumulates silently. Consecutive night shifts compound cognitive depletion even when physical workload feels manageable.
This is why doctors often feel worse on the third or fourth night shift—not better.
Night Shifts, Mental Fatigue, and Medical Errors
Mental fatigue is a known risk factor for clinical errors. Studies published in the BMJ show that sleep deprivation and circadian disruption impair attention, working memory, and judgment.
This is not about effort or professionalism. It is about neurobiology.
Mental Fatigue vs Physical Fatigue During Night Shifts: A Quick Comparison
| Feature | Mental Fatigue | Physical Fatigue |
|---|---|---|
| Primary system | Brain | Muscles |
| Main cause | Cognitive load, circadian disruption | Physical exertion |
| Prominent in night shifts | Yes | Less so |
| Fixed by sleep alone | No | Often |
| Risk to patient safety | High | Lower |
How Doctors Can Reduce Mental Fatigue During Night Shifts
Reduce Cognitive Load During Night Shifts
-
Use structured checklists
-
Standardize handover templates
-
Avoid unnecessary multitasking
Mental fatigue worsens when decision-making is chaotic.
Protect Post–Night Shift Recovery
-
Avoid bright morning light immediately after night shifts
-
Create a consistent post-shift wind-down routine
-
Limit stimulating tasks before sleep
These strategies improve cognitive recovery, not just sleep duration.
Recognize When Night Shifts Are the Problem—Not You
If symptoms improve on day shifts and worsen during night shifts, this is not burnout. It is circadian injury.
Mislabeling night shift fatigue as burnout leads doctors to blame themselves instead of addressing the real cause.
Are Night Shifts Sustainable Long-Term for Doctors?
Night shifts are tolerable in short bursts. Long-term exposure without proper recovery increases the risk of:
-
Chronic mental fatigue
-
Burnout
-
Mood disturbances
-
Reduced clinical performance
The goal is not to eliminate night shifts—but to understand their true cost.
Final Thoughts: Night Shifts Drain the Brain Before the Body
Night shifts do not just make doctors tired. They quietly erode mental stamina, judgment, and emotional resilience—often long before physical exhaustion appears.
If you feel mentally exhausted despite adequate sleep, you are not weak. You are experiencing the predictable effects of night shifts on the human brain.
Understanding the difference between mental fatigue vs physical fatigue is the first step toward safer practice, better recovery, and long-term sustainability in medicine.