Night shifts are one of the most misunderstood stressors in medicine. Most doctors believe that if they are disciplined enough—sleep earlier, power through fatigue, drink coffee strategically—they can “handle” night shifts without major consequences. That belief is wrong.
Night shifts do not fail because doctors lack discipline. They fail because rotating schedules force the brain to function against human biology. Many of the sleep problems doctors experience during night shifts are not inevitable—but they are predictable, and often self-inflicted through well-intentioned mistakes.
This article breaks down the most common sleep mistakes doctors make during night shifts, why they backfire, and how to fix them using a physiology-first approach.
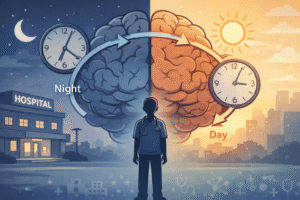
Why Night Shifts Are a Unique Sleep Problem for Doctors
Night shifts are not just “late workdays.” They represent a direct assault on the circadian rhythm—the internal clock that regulates sleep, hormones, body temperature, and cognitive performance.
Unlike fixed night workers, doctors on rotating night shifts never fully adapt. Just as the body starts adjusting, the schedule flips again. This creates a state similar to chronic jet lag, except there is no recovery window.
During night shifts:
-
Melatonin secretion is suppressed
-
Cortisol rhythms become disordered
-
Sleep pressure and circadian timing fall out of sync
-
Cognitive performance declines even if total sleep hours look “adequate”
Understanding this mismatch is critical, because many sleep mistakes doctors make during night shifts are attempts to force normal sleep onto an abnormal biological situation.
Common Sleep Mistakes Doctors Make During Night Shifts
Mistake #1: Trying to Maintain a “Normal” Sleep Schedule During Night Shifts
Many doctors attempt to keep a daytime sleep schedule while working night shifts, believing this preserves normality. In reality, it creates constant circadian conflict.
The brain cannot be awake at night and sleep normally during the day without consequences. This approach leads to fragmented sleep, persistent fatigue, and poor recovery between shifts.
Why it fails:
Your circadian rhythm does not negotiate. Partial compliance results in partial dysfunction.
Mistake #2: Going to Bed Early Before Night Shifts
This is one of the most common and damaging mistakes during night shifts. Doctors feel tired, so they go to bed early “to prepare.”
What happens instead:
-
Sleep pressure is insufficient
-
The brain stays alert
-
Time in bed increases anxiety
-
Insomnia patterns develop
Why it fails:
Fatigue is not the same as sleep pressure. Exhaustion does not guarantee sleep.
Mistake #3: Treating Exhaustion as Sleep Pressure after Night Shifts
After night shifts, doctors often feel physically drained but mentally wired. They lie in bed expecting sleep that never arrives.
Sleep pressure is driven by time awake—not by how tired you feel. When doctors confuse these two signals, they repeatedly fail to fall asleep and unintentionally train the brain to associate bed with frustration.
Mistake #4: Poor Light Management After Night Shifts
Light exposure is the most powerful circadian signal. Many doctors finish night shifts and expose themselves to bright morning light without realizing they are actively shutting down melatonin production.
This makes post-shift sleep shorter, lighter, and less restorative.
Why it fails:
Light is not neutral. Morning light tells your brain it is daytime—whether you want it to or not.
Mistake #5: Incorrect Caffeine Timing During Night Shifts
Caffeine is often used reactively during night shifts. Doctors drink it when they feel tired, without considering timing or half-life.
Caffeine can remain active for 6–8 hours. Poor timing leads to:
-
Delayed sleep onset
-
Reduced deep sleep
-
Incomplete recovery before the next shift
Used incorrectly, caffeine worsens long-term night shift sleep problems.
Mistake #6: Using Melatonin Without a Strategy During Night Shifts
Melatonin is frequently misunderstood. It is not a sleeping pill—it is a circadian signal.
Many doctors take melatonin at random times or in excessive doses after night shifts, expecting sedation. This often produces minimal benefit or worsens circadian confusion.
Why it fails:
Melatonin works only when timing aligns with circadian phase—not when taken reactively.
Mistake #7: Avoiding Strategic Naps During Night Shifts
Some doctors avoid naps because they fear it will ruin “proper sleep” later. During night shifts, this logic collapses.
Short, planned naps can:
-
Improve alertness
-
Reduce medical error risk
-
Preserve cognitive function
Unplanned exhaustion naps, however, often backfire.
Mistake #8: No Structured Recovery After Night Shifts
After the final night shift, many doctors either sleep all day or push through exhaustion without a plan. Both extremes delay circadian recovery.
Without a structured reset, sleep debt accumulates across rotations, leading to chronic fatigue and burnout.
How to Fix Sleep Problems During Night Shifts
Anchor Sleep Instead of Chasing Perfect Sleep During Night Shifts
During night shifts, the goal is not perfect sleep—it is protected anchor sleep.
Anchor sleep means preserving a consistent 3–4 hour block of uninterrupted sleep across workdays. This stabilizes circadian signals and reduces cumulative sleep debt.
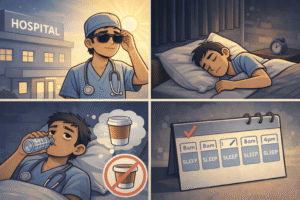
Use Light Strategically on Night Shifts
-
Seek bright light exposure during the night shift when alertness is needed
-
Aggressively limit light exposure after the shift (sunglasses, screen avoidance)
-
Allow daylight exposure only when resetting after the final night shift
This approach aligns circadian cues instead of fighting them.
For a detailed breakdown of light and circadian timing, see the Sleep Foundation’s overview of circadian rhythm disorders.
Smarter Caffeine Use During Night Shifts
-
Take caffeine early in the shift
-
Avoid caffeine in the final 6–8 hours before planned sleep
-
Use smaller, timed doses rather than large boluses
Caffeine should support performance—not sabotage recovery.
Reset Properly After the Last Night Shift
After the final night shift:
-
Sleep a short recovery block (3–4 hours)
-
Wake up and get daylight exposure
-
Avoid long daytime sleep
-
Return to a normal bedtime that evening
This prevents prolonged circadian drift.
Why Generic “Sleep Hygiene” Fails for Night Shifts
Most sleep advice assumes a stable circadian rhythm. Night shifts violate that assumption.
Telling doctors to “go to bed earlier,” “avoid naps,” or “just be consistent” ignores biological reality. Night shift sleep is not a discipline problem—it is a physiology problem.
Long-Term Consequences of Poor Night Shift Sleep
Repeated sleep disruption from night shifts is associated with:
-
Cognitive impairment
-
Mood disturbances and burnout
-
Metabolic dysfunction
-
Cardiovascular risk
These outcomes are not personal failures. They are predictable consequences of unmanaged circadian disruption.
Final Thoughts: Night Shifts Are a Biological Challenge, Not a Personal Weakness
Doctors often blame themselves when night shifts feel unbearable. That blame is misplaced.
Night shifts are difficult because they contradict human biology—not because doctors are weak or undisciplined. Once sleep mistakes are recognized and corrected, performance improves, recovery becomes possible, and night shifts stop feeling like a personal failure.
You do not need more willpower. You need a better strategy.






1 comment
Thanks lots for sharing 😊