Telemedicine is aggressively marketed to doctors as the ultimate solution to burnout, low pay, and geographic restriction. Social media posts promise flexible schedules, remote doctor jobs, and the ability to earn from anywhere in the world. For doctors working abroad, international medical graduates, and physicians waiting for exams or registration, telemedicine often looks like the perfect escape.
The truth is more complicated.
Telemedicine can be useful for doctors abroad—but only in specific situations, under strict legal boundaries, and with realistic expectations. Many doctors enter telemedicine expecting freedom and financial upside, only to encounter licensing barriers, low pay, clinical risk, and a different kind of burnout.
This article breaks down the real opportunities and hard limits of telemedicine for doctors abroad, without hype. If you are considering telemedicine jobs, online doctor work, or telehealth opportunities as a physician working overseas, this guide will help you decide whether telemedicine is a smart move—or a costly distraction.
What Telemedicine Actually Means for Doctors Today
Telemedicine is not a single job type. It is an umbrella term covering multiple clinical and non-clinical roles, each with different requirements and risks.
For doctors, telemedicine usually falls into four categories:
-
Synchronous telemedicine: live video or audio consultations
-
Asynchronous telemedicine: chat-based or message-based consultations
-
Tele-triage and advice services: risk assessment and referral guidance
-
Non-clinical telemedicine roles: clinical review, utilization management, digital health support
Most telemedicine jobs advertised to doctors abroad fall into the lower-autonomy, high-volume end of this spectrum. Understanding this early prevents disappointment.
Why Telemedicine Is So Attractive to Doctors Abroad
Telemedicine appeals strongly to doctors working outside their home country for several reasons.
Telemedicine as a Temporary Career Bridge
For many international doctors, telemedicine looks like a way to:
-
Earn income while preparing for licensing exams
-
Maintain clinical engagement during career transitions
-
Supplement hospital income with online consultation jobs
-
Reduce reliance on night shifts or overtime
In theory, telemedicine offers flexibility and geographic independence. In practice, those benefits are conditional.
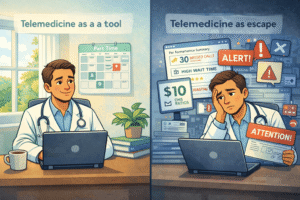
The Psychological Pull of Telemedicine
Telemedicine promises control: control over time, location, and workload. For doctors who feel trapped by rigid hospital systems, this is deeply appealing. However, control in telemedicine is often limited by platform rules, performance metrics, and legal constraints.
The Real Telemedicine Opportunities for Doctors
Despite its limitations, telemedicine does offer genuine opportunities when used strategically.
Telemedicine as a Part-Time Income Supplement
For doctors with appropriate licensing, telemedicine can function well as a side income. It works best when treated as a supplement rather than a primary job. Many doctors use telemedicine to smooth income variability or fund exam preparation.
Skill Development Through Telemedicine
Telemedicine improves:
-
Clinical communication
-
Risk stratification
-
Decision-making with limited data
These skills transfer well to emergency medicine, primary care, and remote settings.
Entry Into Digital Health Through Telemedicine
Some doctors use telemedicine roles to transition into:
-
Digital health advisory positions
-
Clinical quality assurance
-
Medical protocol development
These roles are less visible but often more sustainable.
Telemedicine Licensing and Legal Reality for Doctors Abroad
This is where most doctors underestimate the complexity of telemedicine.
Telemedicine Jurisdiction Rules
In telemedicine, the patient’s location determines jurisdiction, not the doctor’s. If you provide telemedicine care to a patient in a specific country or state, you are usually required to hold valid registration in that jurisdiction.
This principle is outlined by major regulators and organizations, including the World Health Organization (WHO).
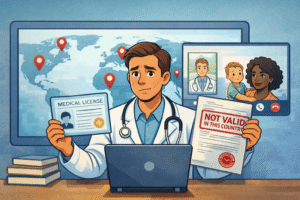
Registration Requirements for Telemedicine Doctors
Most telehealth platforms require:
-
Full medical registration
-
Proof of current practice
-
Local malpractice coverage
For international medical graduates, this often creates a bottleneck. Platform approval does not override legal licensing requirements.
Malpractice and Liability in Telemedicine
Telemedicine shifts clinical risk, not responsibility. Doctors remain accountable for their advice, even when working under platform protocols. Misunderstanding this is one of the most dangerous mistakes doctors make when entering telemedicine.
Telemedicine Income Reality: What Doctors Actually Earn
Income expectations around telemedicine are often unrealistic.
Common Telemedicine Pay Models
-
Pay-per-consultation
-
Hourly rates with performance targets
-
Subscription or package-based models
Rates vary widely but are generally lower than in-person clinical work when adjusted for time and cognitive load.
Why Telemedicine Pay Disappoints Many Doctors
-
High patient volume
-
Strict consultation time limits
-
Unpaid administrative work
Doctors who earn well in telemedicine usually have local licenses, niche expertise, or hybrid roles.
Hidden Downsides of Telemedicine for Doctors
Telemedicine has its own form of burnout.
Cognitive Fatigue in Telemedicine
Back-to-back telemedicine consultations allow little mental recovery. Decision fatigue accumulates faster than in traditional clinics.
Defensive Medicine Pressure in Telemedicine
Without physical exams, doctors often compensate by:
-
Over-referring
-
Over-advising
-
Practicing conservatively
This reduces professional satisfaction and increases stress.
Loss of Clinical Fulfillment
Many doctors report that long-term telemedicine work feels transactional and detached, particularly in chat-based models.
Telemedicine for International Medical Graduates (IMGs)
Telemedicine is often marketed heavily to IMGs, but access is limited.
What Telemedicine Looks Like for IMGs
-
Fewer platform approvals
-
Accent and communication bias
-
Limited advancement
Most IMGs who succeed in telemedicine use it temporarily, not as a long-term career.
Strategic Use of Telemedicine for IMGs
Telemedicine works best for IMGs as:
-
A short-term income bridge
-
A skill-maintenance tool
-
A complement to traditional clinical work
It is rarely a replacement.
Who Telemedicine Is Actually Good For
Telemedicine suits doctors who:
-
Are legally registered in target jurisdictions
-
Have strong communication skills
-
Prefer structured, protocol-driven work
-
Can emotionally detach from outcomes
Who Should Avoid Telemedicine
Doctors who value diagnostic certainty, long patient relationships, or procedural work often find telemedicine unsatisfying.
The Future of Telemedicine for Doctors Abroad
Telemedicine is becoming more regulated, not more open. Cross-border telemedicine is under increasing scrutiny. Automation and AI-assisted triage are expanding, while entry-level doctor roles are narrowing.
Professional bodies such as the American Medical Association continue to emphasize licensing and accountability in telemedicine practice.
Doctors who approach telemedicine strategically will benefit. Those chasing hype will struggle.
Final Verdict: Is Telemedicine Worth It for Doctors Abroad?
Telemedicine is not a shortcut, a loophole, or an escape from medicine. It is a tool.
Used wisely, telemedicine can provide flexibility, supplemental income, and career leverage for doctors abroad. Used blindly, it leads to frustration, legal risk, and burnout.
The smartest doctors treat telemedicine as one component of a broader career strategy—not the destination itself.
One Last Reality Check
If telemedicine sounds too good to be true, it usually is. If it sounds boring but stable, that’s where the real value often lies.